Familial hypercholesterolemia (FH) is a genetic disorder that significantly increases the risk of early-onset cardiovascular disease, including heart attacks, strokes, and coronary artery disease (CAD). As a result, early detection is crucial, as undiagnosed FH can lead to life-threatening cardiovascular events. Therefore, identifying individuals at risk becomes essential for preventing severe outcomes. Genetic testing for familial hypercholesterolemia has emerged as a powerful tool, enabling earlier detection, more effective intervention, and personalized treatment strategies. By analyzing specific genes associated with LDL, HDL, and triglyceride (TGL) metabolism, healthcare providers can offer more targeted care that reduces long-term cardiovascular risk.
Fortunately, with the advancement of genetic testing, healthcare providers now have the means to identify at-risk individuals earlier in life, paving the way for proactive management and better health outcomes. By leveraging genetic insights, clinicians can make more informed decisions about patient care, implement early interventions, and dramatically reduce the risks associated with FH. In this blog, we explore the importance of genetic testing for FH, and key genes related to LDL, HDL, and triglyceride (TGL) metabolism, can help in early detection and personalized treatment strategies.
Understanding Familial Hypercholesterolemia
FH causes high levels of low-density lipoprotein (LDL) cholesterol and, in some cases, elevated triglycerides. The condition leads to cholesterol accumulation in arterial walls, triggering early atherosclerosis and increasing the risk of CAD. While lipid profile measurements and clinical criteria, such as the Dutch Lipid Clinic Network Criteria, can help diagnose familial hypercholesterolemia (FH), genetic testing provides a more definitive approach to identifying at-risk individuals. Furthermore, genetic testing is particularly valuable for detecting FH in individuals who may not meet traditional diagnostic thresholds. By transitioning from standard assessments to genetic analysis, healthcare providers can gain a clearer understanding of a patient’s genetic risk, enabling earlier intervention and personalized treatment. This shift allows clinicians to implement more precise care strategies and significantly reduce long-term cardiovascular risk. In summary, genetic testing bridges the gap between clinical indicators and personalized healthcare, offering a more accurate and comprehensive method for FH diagnosis.
The genetic mutations responsible for FH predominantly affect genes involved in lipid metabolism and cholesterol homeostasis. The most well-known genetic cause of FH is mutations in the LDLR gene, which encodes the low-density lipoprotein receptor. However, several other genes have been implicated in FH or are associated with variations in lipid levels and atherosclerosis risk. Understanding these genetic factors enables clinicians to provide personalized care and intervention strategies.
Key Genes
A comprehensive genetic test for FH typically examines a variety of genes known to impact cholesterol metabolism and cardiovascular risk. The following genes are included in our genetic panel:
- LDLR (Low-Density Lipoprotein Receptor): Mutations in LDLR are the most common cause of FH. These mutations reduce the number or function of LDL receptors on liver cells, leading to decreased clearance of LDL cholesterol from the bloodstream. This results in elevated LDL levels and an increased risk of atherosclerosis.
- APOB (Apolipoprotein B): APOB encodes the primary protein component of LDL particles. Mutations in APOB impair LDL particle function, reducing liver clearance efficiency and raising cholesterol levels.
- APOC4 (Apolipoprotein C-IV): This gene influences lipid metabolism by modulating lipoprotein activity, including triglyceride-rich particles. Variations in APOC4 increase the risk of atherosclerotic cardiovascular disease (ASCVD) due to altered lipid processing.
- CELSR2 (Cadherin EGF LAG Seven-Pass G-Type Receptor 2): This gene regulates lipids and impacts atherosclerosis risk. Abnormalities in CELSR2 alter lipid profiles and raise CAD risk, though researchers continue to study its role.
- LIPC (Hepatic Lipase): LIPC plays a crucial role in breaking down lipoproteins. Mutations in LIPC disrupt LDL and HDL cholesterol balance, worsening atherosclerotic risk.
- ABCA1 (ATP-Binding Cassette Subfamily A Member 1): ABCA1 facilitates cholesterol efflux from cells, maintaining HDL cholesterol levels. Mutations impair cholesterol clearance, elevating LDL and lowering HDL cholesterol.
- GCKR (Glucokinase Regulator): GCKR regulates glucose and lipid metabolism. Variations in GCKR disturb lipid profiles, particularly by raising triglyceride levels.
- APOA5 (Apolipoprotein A-V): APOA5 plays a vital role in triglyceride metabolism. Mutations in APOA5 lead to elevated triglyceride levels, significantly heightening cardiovascular risk.
Clinical Benefits of Genetic Testing for FH
Genetic testing for FH provides a wealth of information that can improve patient management in several ways:
- Early Detection: FH often goes undiagnosed until a patient experiences a cardiovascular event. Genetic testing allows for early identification of affected individuals, enabling interventions before the onset of clinical symptoms or complications.
- Personalized Treatment Plans: Genetic insights enable healthcare providers to tailor treatment strategies based on the patient’s specific genetic mutations. For example, patients with certain LDLR mutations may require more aggressive statin therapy or LDL apheresis, while others with APOB mutations might benefit from specific targeted therapies.
- Family Screening: FH is an autosomal dominant disorder, meaning that family members of affected individuals have a 50% chance of inheriting the condition. Genetic testing can identify at-risk family members, allowing for early interventions and reducing the burden of cardiovascular disease within families.
- Better Outcomes: When patients are identified early and treated appropriately, the progression of atherosclerosis can be slowed, reducing the risk of premature cardiovascular events. Early interventions, such as lifestyle modifications and statin therapy, are more effective when initiated before significant arterial damage occurs.
Conclusion
Genetic testing for familial hypercholesterolemia revolutionizes lipid disorder management by enabling personalized care and early interventions. By identifying genetic mutations, clinicians can diagnose at-risk individuals who might otherwise remain undetected, reducing cardiovascular risk and improving long-term outcomes. This proactive approach allows for timely, targeted treatments, enhancing overall patient health and well-being.
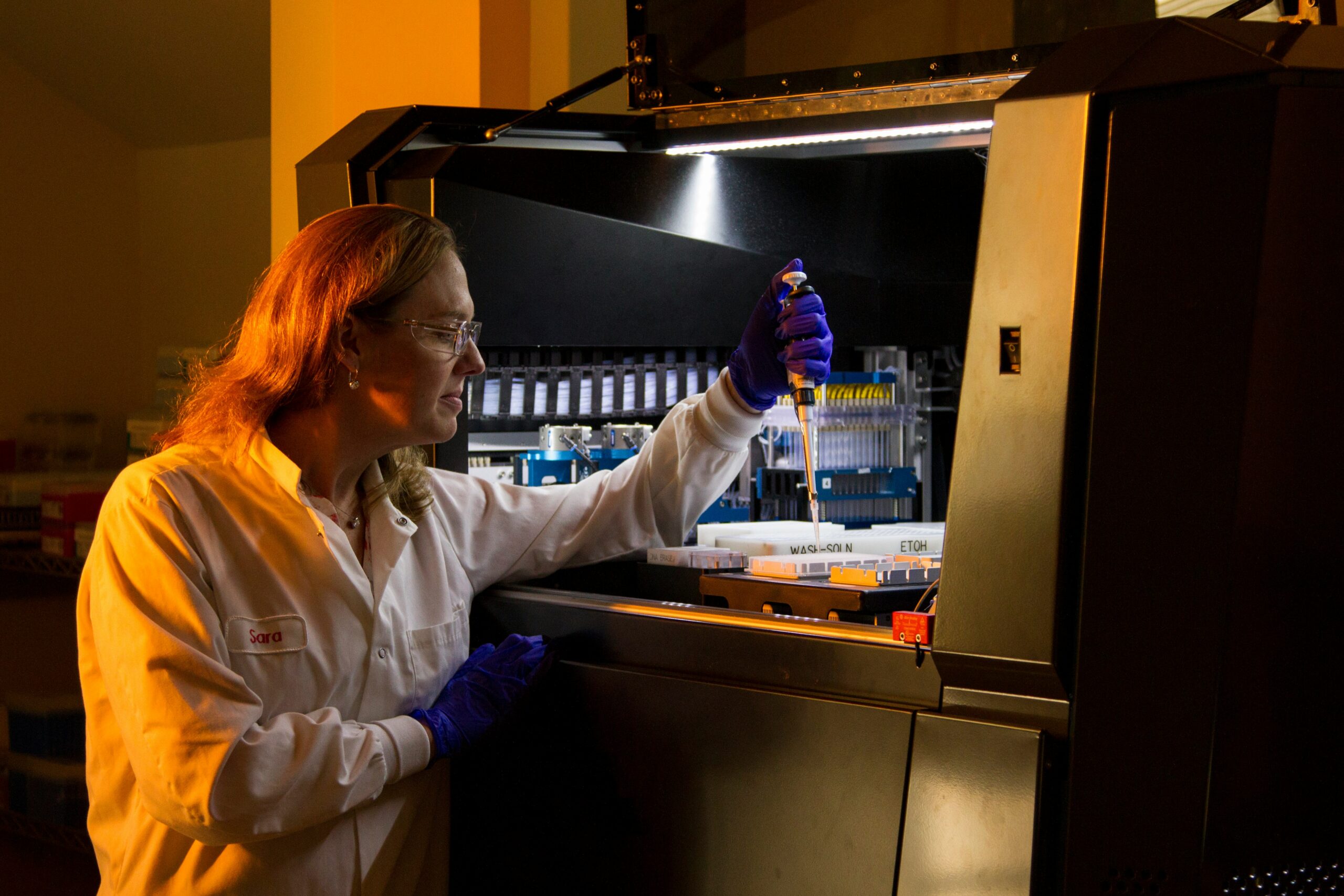
At ExtendingMe, we provide a Foundational Panel that examines essential genes involved in lipid metabolism. This service equips clinicians with the resources necessary for early detection, precise diagnosis, and tailored treatment plans for patients with FH.
Ensure early and accurate diagnosis for your patients by enabling personalized interventions and improving long-term cardiovascular outcomes.
