Healthcare providers are constantly navigating the upstream drivers of chronic disease and two mechanisms keep showing up at the center of it all: mitochondrial dysfunction and inflammation. These aren’t isolated issues, in fact, they’re tightly interlinked. When mitochondrial health declines, inflammation flares. And when inflammation persists, it further damages mitochondria. It’s a vicious cycle that is reflected in everything from metabolic syndrome and autoimmune conditions to neurodegenerative disease.
Understanding the relationship between mitochondrial dysfunction and inflammation isn’t just academic, it’s clinically actionable. The mitochondria aren’t just about energy production anymore, they’re key players in immune signaling, redox balance, and even cell survival. When they fail, the fallout extends far beyond energy metabolism.
In the clinical setting, identifying early signs of mitochondrial stress and addressing them can shift the trajectory of disease especially in patients with genetic susceptibilities. Let’s look at five mitochondrial genes that are particularly relevant to this conversation.
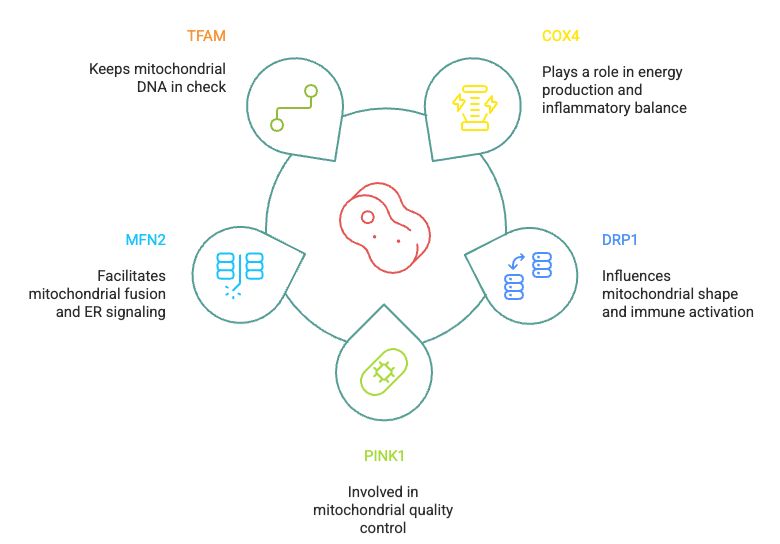
1. COX4: Energy Production and Inflammatory Balance
The COX4 gene encodes a key subunit of Complex IV in the mitochondrial electron transport chain. When COX4 is underexpressed or functionally impaired, ATP production stalls, and oxidative stress ramps up. That excess ROS doesn’t just damage mitochondria, it also activates inflammatory pathways, including NF-κB and the NLRP3 inflammasome. For patients with chronic fatigue, cardiometabolic issues, or unexplained inflammation, COX4 variants may offer an overlooked clue.
2. DRP1: Mitochondrial Shape and Immune Activation
DRP1 regulates mitochondrial fission, a process essential for quality control. But when DRP1 is overactive, mitochondria become excessively fragmented, making them less efficient and more prone to releasing mitochondrial DNA into the cytosol. That mtDNA acts as a danger signal, triggering innate immune responses. Inflammatory conditions like IBD and neuroinflammation have been linked to elevated DRP1 activity.
3. PINK1: Mitochondrial Quality Control
PINK1 is a key initiator of mitophagy, the selective removal of damaged mitochondria. When PINK1 isn’t functioning well, dysfunctional mitochondria accumulate and act as chronic sources of ROS and inflammatory signals. This has been well documented in neurodegenerative diseases, particularly Parkinson’s, but also has broader relevance in aging and chronic inflammation. Supporting PINK1 pathways may be one way to reduce inflammatory burden in high-risk patients.
4. MFN2: Mitochondrial Fusion and ER Signaling
MFN2 helps maintain mitochondrial integrity and ensures communication between mitochondria and the endoplasmic reticulum. Low levels of MFN2 have been associated with insulin resistance, hepatic inflammation, and even cardiac dysfunction. From a clinical perspective, assessing MFN2 function may be especially relevant in patients with metabolic inflammation or non-alcoholic fatty liver disease.
5. TFAM: Keeping Mitochondrial DNA in Check
The TFAM (Transcription Factor A, Mitochondrial) gene plays a vital role in maintaining and regulating mitochondrial DNA (mtDNA). It is essential for both the replication and transcription of mtDNA and helps package mitochondrial DNA into organized structures called nucleoids. Through these functions, TFAM supports healthy mitochondrial biogenesis and energy production. Variants in this gene have been linked to mitochondrial dysfunction, which can contribute to aging, neurodegenerative diseases like Parkinson’s and Alzheimer’s, and metabolic disorders. TFAM is considered a master regulator of mitochondrial function, especially under cellular stress.
At Extending Me, we analyze key genes involved in mitochondrial health, including COX4, DRP1, PINK1, MFN2, and TFAM, to assess an individual’s predisposition to mitochondrial dysfunction and inflammation. This allows health care professionals to go beyond generic advice and provide personalized recommendations that align with each patient’s unique genetic and biochemical profile. Depending on the individual’s risk, we tailor interventions across nutrition (e.g., mitochondrial-supportive nutrients), lifestyle (e.g., circadian optimization, movement strategies), targeted supplementation, and lab testing (e.g., organic acids, oxidative stress markers, mitochondrial metabolites). This integrative, gene-informed approach can help health care providers support mitochondrial resilience and inflammatory balance with greater clinical precision.
Clinical Takeaways
Practitioners often focus on inflammation as the end result. But mitochondrial dysfunction and inflammation often go hand in hand and mitochondrial health may be the starting point. Identifying patients with genetic variants in COX4, DRP1, PINK1, MFN2, or TFAM can help guide more targeted interventions.
This mitochondria-inflammation axis is a therapeutic lever one that’s both measurable and modifiable.
